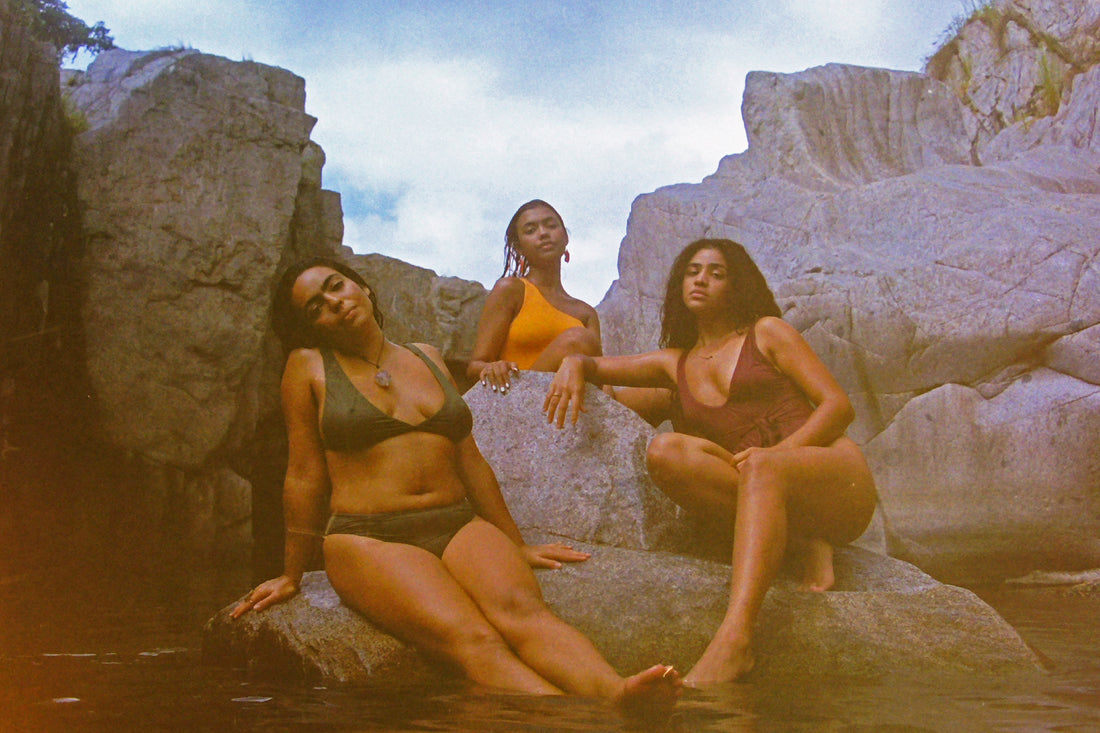
Facing Misdiagnoses: BIPOCs & Trans Folks Take Sexual Health Into Their Own Hands
Share
Medicine and profit are related. Now more than ever, we see a system where medical school and health care organizations are often funded by pharmaceutical companies or politically motivated businesspeople. The system of corporations that finance health care services for profit is called the medical industrial complex, and it has led many to feel that as long as money runs medicine, the people we trust to keep us healthy will value profit over their patients. It follows that within this system, racism and Transphobia persist, since these minority populations are intentionally neglected by every other aspect of this country’s economy.
Professionals in sexual healthcare hold a uniquely important role. Not only are they tasked with preserving our health, but they handle our concerns around some of our most stigmatized body parts and human functions. These stigmas are amplified for BIPOCs and Trans folks. Many members of marginalized groups feel that their doctors, their gynecologists, urologists, and other sexual health specialists fall short because of their lack of knowledge and biases. This is where a specific pattern emerges: the negative experiences BIPOCs and Trans people have with sexual health professionals often leads these patients to distrust their doctors and seek alternatives, specifically self treatment.
The negative experiences BIPOCs & Trans people have with sexual health professionals often leads to patient distrust & seeking alternative self-treatment.
“It’s a true and unacceptable fact that BIPOC and trans patients are some of the least well treated medically,” says Marieme Mbaye, MD, a gynecologist and women's health specialist in New York City. “This stems not only from the inherent biases that exist in our society but also from the lack of training in medicine about issues involving these vulnerable populations. Many providers want to be able to provide quality healthcare to all of our patients, but the sad fact is that unfair insurance policies and prohibitive laws, especially surrounding women’s bodies, often limit what can be offered.”
BIPOCs at the Doctors
There is an extensive history of medical racism in this country, both generally and with sexual health specifically, and it is genuinely frightening the extent to which racial stereotyping persists to this day. In every field, too many medical students are graduating with the notion that darker skinned people feel less pain, that they have thicker skin.
In regards to sexual health, a study published by the American Journal of Obstetricians and Gynecologists found that racial biases affect birth control recommendations. Black and Latinx people with uteruses in the study were more likely to have long term birth control methods such as IUDs recommended for them, as opposed to shorter term methods like the pill. This likely circles back to stereotypes about BIPOCs being generally “less responsible” and therefore more at risk for unwanted pregnancy. Conversations about contraceptives are just the beginning.
Statistics are readily available about the racial disparities in sexual health outcomes such as fetal deaths and maternal deaths. Black and Indigenous women are up to three times as likely to die during childbirth than white women, and Black women are twice as likely to experience their fetus dying. Some of these disparities can be attributed to distinct stressors oppressed peoples face, such as experiencing prejudice and discrimination, or a lack of social and institutional support. But, according to the American College of Obstetricians and Gynecologists, “some remain because of factors at the patient, health care system, and practitioner levels.” A large contributor is the poorer quality of care black women receive, and that care is often denied to them when they report being in pain.
Implicit bias training in medical schools is intended to cover topics as broad as race, fatphobia, disability and more often within the span of weeks, as opposed to months or years. Judging by the degree to which medical racism exists, they are clearly not effective enough. “I can honestly only remember a few very brief, and largely inadequate, lectures touching on racism and bias in medicine throughout my 8 years of training.” says Dr. Mare.
The result of individuals continuing through their studies with their biases unchecked? When those individuals become doctors, black and brown people leave their appointments feeling unheard and belittled. As far as sexual health, this means that BIPOCs are not informed of all of their birth control options; they are not screened for preterm birth. They are at risk for misdiagnosis, which puts them at risk for incorrect treatment recommendations. It all adds up to an abundance of patient distrust.
Trans People at the Doctors
From grade school sex education, to “birds and bees” conversations between parents and children, all the way to the doctors office, Trans people are excluded from most conversations about sex. And though there is no universal Trans sexual experience, the possibilities of experiencing stigma, social bias, embarrassment, stress, a pressure to remain stealth, and/or a fear of rejection can influence sexual interactions and one’s sense of self.
The history of Trans health care, too, has been tainted, specifically by dangerous experiments that took advantage of the Trans population and stigmatizing psychological diagnoses which have acted as obstacles to accessing physical and sexual care. Today, “the biggest barrier to health care reported by Transgender individuals is lack of access due to lack of providers who are sufficiently knowledgeable on the topic,” according to NCBI.
Trans health literacy is required by very few hospitals in the US. Many well intentioned healthcare workers may not even know where to start these conversations, especially considering that the majority of Trans people surveyed in 2015 said that not all of their healthcare professionals even knew they were Trans in the first place because of the stigma that keeps people from being comfortable enough to divulge this information.
Not all of their healthcare professionals even knew they were Trans in the first place because of the stigma that keeps people from being comfortable enough to divulge this information.
Sexual health related appointments lack a few things in particular. There are psychological concerns when it comes to sex that are not addressed. The CDC’s recommended talking points for clinical sexual health visits do not contain any discussion on the pronouns one identifies with, or language one may prefer to use for their genitals. There is also no push to get doctors to ask patients about their use of prosthetics or toys, their relationship types (ie. monogamous, poly, etc.), or their pleasure and satisfaction. There is an over-validation of high risk sexual activities such as PIV (penis in vagina) or anal sex, and under-validation of other things someone might deem “sex” like oral sex, or toy play.
A Trans health literate provider would not only be able to address the above-mentioned psychological concerns, but would also know to discuss with patients how synthetic hormones change erectile functions, clitoral growth and sensitivity, ability to self-lubricate, one’s sexual desire and more. Gender affirming surgeries, of course, carry their own changes to sexual functioning, so it's of notable value that professionals in sexual healthcare be competent enough to initiate these discussions with patients who undergo these procedures.
“As someone who values and wants to support the Trans community, it can be frustrating to see how often that community is overlooked and left out of important conversations about counseling, diagnosis and treatment of common things.,” Dr. Mare added.
In talking to the Fenway Trans Health Program, one Trans male patient recounted having vaginal pap smears taken despite having told their doctor that they had anal sex with both cis and Trans men rather than vaginal sex. Months later, another doctor told them that in order to do STI testing, they needed to have an anal pap smear performed as opposed to a vaginal one. This is just one example of a lack of training leading to confusion around testing, and ultimately affecting decisions on what one may or may not be treated for.
Alternatives to Western Medicine: Holistic Healing
Harmful doctor visits for members of the BIPOC and Trans community are caused by a lack of training and internalized biases. Since this has become—or rather always been—the norm, it is only logical that people have begun to look for less conventional solutions to their problems.
Within both of these populations, in addition to many other marginalized communities, holistic healing has a newfound popularity. Holistic healing is an umbrella term for practices that incorporate healing for the whole self: mind, body and soul, upheld by an understanding that the body is self-healing. It is affiliated with treatment alternatives to medicating one’s symptoms, such as diet, exercise, psychological counseling, acupuncture, and more.
For Indigenous, Black, and Latinx folks, many holistic practices may represent a return to one’s roots, since historically these groups utilized holistic healing ideals before colonization. For the Trans population who experience anxiety, depression, and stress at high rates, the mind-body connection may be particularly helpful in understanding physical ailments. The accessibility and affordability of holistic healing allows many people to feel like it is approachable for them, and that with some research, they can take their health into their own hands.
Holistic sexual wellness, in particular, takes into account sexual traumas which remain in the mind and body far beyond the moment they are first experienced. It factors in individual preferences, past experiences, marginalized identities, the psychological and medical concerns of those with STIs, and one’s mental state outside of the bedroom. If you strip it down, holistic healing at its core is about prioritizing the wellbeing of one’s entire person, rather than being able to profit from treating symptoms alone.
“I grew up knowing many extended family members who mostly relied on holistic medicine for their health so I’ve never been a stranger to it,” Dr. Mare told us. “But just like Western medicine, holistic medicine can and should be vigorously studied when possible. There are some very reasonable alternatives available but even within the holistic umbrella, trying to follow evidence-based methods is important to avoid harm.”
At its core, holistic healing is about prioritizing the wellbeing of one’s entire person, rather than being able to profit from treating symptoms alone.
Critiqued for being relatively dangerous, within the Trans community there has been something called “DIY” Transitioning. Through this, Trans folks, barred from receiving gender affirming care, look to the black market for hormones. Simply labeling this behavior as risky, though, might serve to over-legitimate our healthcare system which, as previously discussed, has been corrupt throughout history. DIY treatments are understudied, but believed to be relatively common.
Both holistic health and “doing it yourself” alternatives feel like the only option to many because of the way medicine in this country looks now, and the insufficient solutions to BIPOC and Trans sex-related concerns that doctors provide. Both of these phenomena show a migration towards self-treatment. Critics are quick to label holistic healing a hoax, and DIY methods unsafe. Regardless of which side of these debates are in the right, the real problem that should take center stage is that non-racist, Trans-competent care is not currently available. People feel they need to be self reliant because they cannot rely on a system that’s emphasis on profit overshadows it’s self proclaimed intention: helping people.
Related Reading
The Intersection of Sexual and Mental Health
LGBTQIA & Z the Bug Interview with Z the Bug
Redefining Activism by Kenta Ch’umil
Race, Gender, and American Gynecology by Dr. Deirdre Cooper Owens
Meet the Author
 |
Tara Michaela (she/her) @tara.michaela is a sex educator, writer, and content creator. Her favorite products Salve and Tonic. "I love Salve because it definitely did the most to get rid of symptoms from yeast infections, but I think Tonic is slept on — it's so multipurpose! I use it for ingrown hairs around my vulva, any dry patches of skin, on my face after doing face masks, on my hair if I straighten it or have a weave, AND it makes my baths super shiny and smell amazing." |
Momotaro Apotheca and its materials are not intended to treat, diagnose, cure or prevent any disease. All material on Momotaro Apotheca is provided for educational purposes only. Always seek the advice of your physician or another qualified healthcare provider for any questions you have regarding a medical condition

1 comment
As a BIPOC queer health provider who emphasizes the importance of noninstitutionalized healing practices for BIPOC folks and specializes in transgender and sex positive health care, I greatly Appreciate this post. I also want to contribute by saying there is still importance in cervical cancer screenings for anyone with a cervix despite their practices with genital penetration due to the many ways hpv can be transmitted outside of penetration. However, anal paps are important for those who are engaging in anal receptive sex. We have little data on the age to start those screenings and the interval for prevention due to transphobia and lack of lgbtqi knowledge in health care. However, it’s a conversation worth having with patients in terms of risks and also their desire to continue with routine anal paps or a high resolution digital rectal exam if an abnormal occurs. I am so excited to see more public conversations about these topics and for our communities to push back against harmful practices by medical professionals!!